Cognitive Behavioral Therapy (CBT) has emerged as a powerful and highly effective treatment for depression, offering hope and relief to millions of individuals battling this debilitating mental health condition. In this comprehensive guide, we’ll delve deep into the world of CBT, exploring its principles, techniques, and the transformative impact it can have on those grappling with depression.
Contents
- 1 Understanding Depression
- 2 The Basics of Cognitive Behavioral Therapy
- 3 Cognitive Behavioral Therapy Techniques for Depression
- 4 The Evidence for Cognitive Behavioral Therapy for Depression
- 5 The Cognitive Behavioral Therapy Process for Depression
- 6 Benefits of Cognitive Behavioral Therapy for Depression
- 7 Finding a CBT Therapist
- 8 Potential Drawbacks and Limitations
- 9 Conclusion
Understanding Depression
Depression is more than just feeling sad; it is a complex mental health disorder characterized by persistent feelings of sadness, hopelessness, and a loss of interest or pleasure in previously enjoyed activities.
Depression manifests in a myriad of ways, with symptoms ranging from emotional and psychological to physical and behavioral.
Also, Depression can disrupt every aspect of a person’s life, from their relationships and work to their physical health. Understanding the severity of this impact underscores the importance of effective treatment.
The Basics of Cognitive Behavioral Therapy
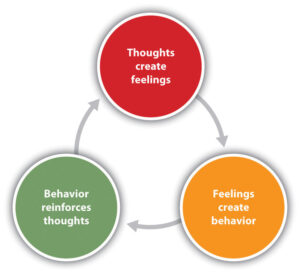
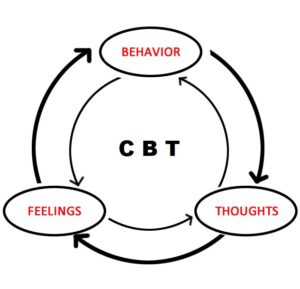
At its core, CBT seeks to identify and modify negative thought patterns and behaviors contributing to depression.
CBT is divided into two components: cognitive and behavioral. These components work in tandem to bring about positive changes in one’s mental well-being.
CBT is typically administered by trained therapists who guide individuals through the process of self-discovery and change.
Cognitive Behavioral Therapy Techniques for Depression
Here are some key CBT techniques commonly used for depression:
Identifying Negative Thoughts: The first step in CBT for depression is to become aware of your negative thought patterns. This can be done by keeping a thought journal, where you record your thoughts when you’re feeling down. Try to identify recurring negative thought patterns.
Challenging Negative Thoughts:
- Reality Testing: Ask yourself if your negative thoughts are based on facts or assumptions. Are there concrete pieces of evidence to support your thoughts?
- Alternative Thoughts: Try to generate more balanced and realistic alternative thoughts. For example, instead of “I’m a failure,” you might think, “I’ve faced challenges before and overcome them.”
Behavioral Activation:
- Activity Scheduling: Create a daily or weekly schedule of activities that you enjoy or that give you a sense of accomplishment. Even small tasks can help improve your mood.
- Graded Task Assignment: Break larger tasks into smaller, manageable steps to avoid feeling overwhelmed.
Mindfulness and Relaxation Techniques:
- Mindfulness Meditation: Learn mindfulness techniques to stay present and reduce rumination on negative thoughts.
- Progressive Muscle Relaxation: Practice relaxation exercises to reduce physical tension and stress.
Problem Solving:
- Identify Problems: Break down your issues into specific problems that you can address.
- Generate Solutions: Brainstorm potential solutions for each problem.
- Evaluate Solutions: Assess the pros and cons of each solution and choose the most feasible one to implement.
Cognitive Restructuring:
- Cognitive Distortions: Recognize and challenge cognitive distortions like all-or-nothing thinking, catastrophizing, and personalization.
- Core Beliefs: Explore and challenge deep-seated negative beliefs about yourself, others, and the world.
The Evidence for Cognitive Behavioral Therapy for Depression
Numerous studies have demonstrated the effectiveness of CBT in treating depression, making it one of the most evidence-based therapeutic approaches.
CBT boasts high success rates in achieving symptom relief, often in a relatively short time frame.
CBT is frequently compared to other therapeutic approaches, highlighting its unique strengths in treating depression.
The Cognitive Behavioral Therapy Process for Depression
Here is an overview of the CBT process for depression:
- Assessment and Goal Setting:
- Initial Assessment: The therapist conducts an initial assessment to understand the client’s history, current symptoms, and life circumstances. They may use standardized depression assessment tools to measure the severity of depression.
- Goal Setting: Together, the therapist and client set specific, measurable, and realistic goals for therapy. These goals may include reducing depressive symptoms, improving daily functioning, or developing coping strategies.
- Psychoeducation: The therapist educates the client about depression, its causes, and the CBT framework. This helps the client understand the cognitive and behavioral aspects of depression and how they are interconnected.
- Identifying Negative Thoughts: The client learns to recognize and record negative thoughts as they occur. They may use a thought diary or journal to track these thoughts.
- Challenging Negative Thoughts: The therapist helps the client examine and challenge their negative thought patterns. This involves looking for evidence to support or refute these thoughts and developing more balanced, rational, and realistic thinking.
Benefits of Cognitive Behavioral Therapy for Depression
Cognitive Behavioral Therapy (CBT) is one of the most well-researched and effective treatments for depression. It offers a range of benefits for individuals struggling with depression:
- Efficacy: CBT is highly effective in treating depression. Numerous clinical trials and studies have shown that it can lead to significant reductions in depressive symptoms and even full remission for many individuals.
- Evidence-Based: CBT is considered an evidence-based therapy, meaning that its effectiveness is supported by extensive scientific research and clinical trials.
- Structured Approach: CBT provides a structured framework for understanding and managing depression. It offers clear techniques and strategies that help individuals systematically address their symptoms.
- Focused on the Present: CBT is a present-focused therapy that helps individuals identify and change negative thought patterns and behaviors that contribute to their depression. This can lead to more immediate relief from symptoms.
- Skills Development: CBT equips individuals with practical skills to manage their depression, such as identifying and challenging negative thoughts, problem-solving, and behavioral activation. These skills can be used throughout life to prevent or manage relapses.
Finding a CBT Therapist
Finding a qualified Cognitive Behavioral Therapy (CBT) therapist is an important step if you’re considering CBT as a treatment for a mental health concern. Here’s a step-by-step guide on how to find a CBT therapist:
- Assess Your Needs: Determine what specific issues or concerns you want to address through CBT therapy. Knowing your goals and needs will help you find a therapist with the right expertise.
- Consult with a Healthcare Provider: If you have a primary care physician or mental health professional, consult with them first. They can provide referrals to CBT therapists or other mental health specialists.
- Contact Your Insurance Provider: If you have health insurance, contact your insurance provider to inquire about CBT therapy coverage and obtain a list of in-network providers. This can help you narrow down your search and manage costs.
- Search Online Directories: Use reputable online directories and search engines to find CBT therapists in your area. Some popular directories include Mantracare and Therapymantra.
- Read Therapist Profiles: Review therapist profiles to learn about their qualifications, specialties, treatment approaches, and experience with CBT. Look for therapists who have experience treating your specific issue.
Potential Drawbacks and Limitations

While Cognitive Behavioral Therapy (CBT) is an effective and widely used therapeutic approach, it does have some potential drawbacks and limitations. It’s important to be aware of these factors when considering CBT as a treatment option:
- Not a One-Size-Fits-All Approach: CBT is not suitable for everyone or every mental health condition. Some individuals may respond better to other types of therapy, such as psychodynamic therapy or dialectical behavior therapy (DBT).
- Time-Intensive: CBT often requires a significant time commitment. Sessions are typically held weekly, and treatment may last for several weeks or months. This may not be feasible for individuals with busy schedules or those seeking short-term solutions.
- Limited Focus on Past Issues: CBT is primarily focused on the present and future, with less emphasis on exploring deep-rooted, unresolved issues from the past. For some individuals, understanding past experiences may be important for their recovery.
- Requires Active Participation: CBT is a highly collaborative approach that requires active participation from the individual. Success depends on the willingness and ability to engage in homework assignments, thought analysis, and skill-building exercises.
Conclusion
In conclusion, Cognitive Behavioral Therapy is a beacon of hope for those grappling with depression. Its evidence-based techniques, coupled with the expertise of trained therapists, offer a path to recovery and a brighter future. Remember, seeking help is the first step towards reclaiming your life from depression’s grip.
If you are experiencing depression related issues, Online Depression Counseling at TherapyMantra can help: Book a trial Online therapy session.


